I had a chance to listen to a great presentation on pacemakers that I thought I’d share.
Pacemakers are used in patients who have irregular heart rhythms that impact cardiac output. This means that the heart could beat too fast, too slow or irregularly due to blocks and or dysfunction of the heart’s electrical conductivity pathways. Electrical impulses pass through the heart in a rhythmic method and cause the heart to relax and contract. It’s this contraction and relaxation that allows blood to be circulated around the body.
Pacemakers consist of an impulse generator and leads that attach to the myocardium that emit electrical impulses. So for assistance a patient suffering from atrial fibrillation would need a pacemaker that senses that there is not proper contraction from the atrium and as a result send a pulse through to normalize contractions.
Depending on where the abnormality lies, pacemakers can be programmed to pace the chambers of the heart in a single or dual fashion – A –atrium , V- ventricle , AA, VV, AV. A device can initiate an impulse when needed or inhibit it. The new age pacemakers can now initialize a rate response at which the pacemaker can pace. This means that unlike the older devices that paced steadily regardless of the patient’s level of activity or the existence of normal beats; new devices can sense the patient’s level of activity and increase or decrease the heart rate as needed.
I learned that there is careful consideration made to voltage, current, and impedance when it comes to managing a patient’s pacemaker. Prior to my knowledge about pacemakers, assumed that a pacemaker was programmed and when a few years have passed then it’s replaced because the battery would need changing. During the lecture it was outlined that depending on the frequency at which a pacemaker is used and how dependent the patient is on the device, the higher will be the voltage capacity. This ensures that the device is able to function to full capacity up until the battery has to be change and that the device does not stop functioning abruptly. Also, lead integrity needs to be sufficient enough to prevent lead breakage because a broken lead could render the pacemaker incapable of sensing and or pacing.
I found it really interesting to learn that lead tips can have steroids on the end that attaches to the myocardium to prevent inflammation. Also, pacemakers can last up to 14 years before the battery needs to be replaced – a good leap from the 6-10 years mark. A magnet is used to reset a pacemaker and with the advent of clothing with magnet closures instead of regular zippers, this can pose a threat to people with pacemakers. The magnet can put the device back to default setting thus erasing any programming. This can therefore have life threatening outcomes for an unknowing patient. So places like the Bay who sell such clothing have labels advising customers of magnet.
Technological advancement has come a long way in improving longevity, functionality and size of pacemakers. It used to be that one couldn’t have an MRI with pacemaker now it’s possible. In 2011, the very first MRI compatible pacemaker was introduced to the market approved by the FDA. Manufactured by Medtronic, these devices are smaller and have material that protects against the electromagnetic effects of the scanner. This is a wonderful step in improving diagnosis and treatment in patient with pacemakers, which as we know is a contraindication for such a test. I hope one day to do research in the world of pacemakers and electrophysiology.
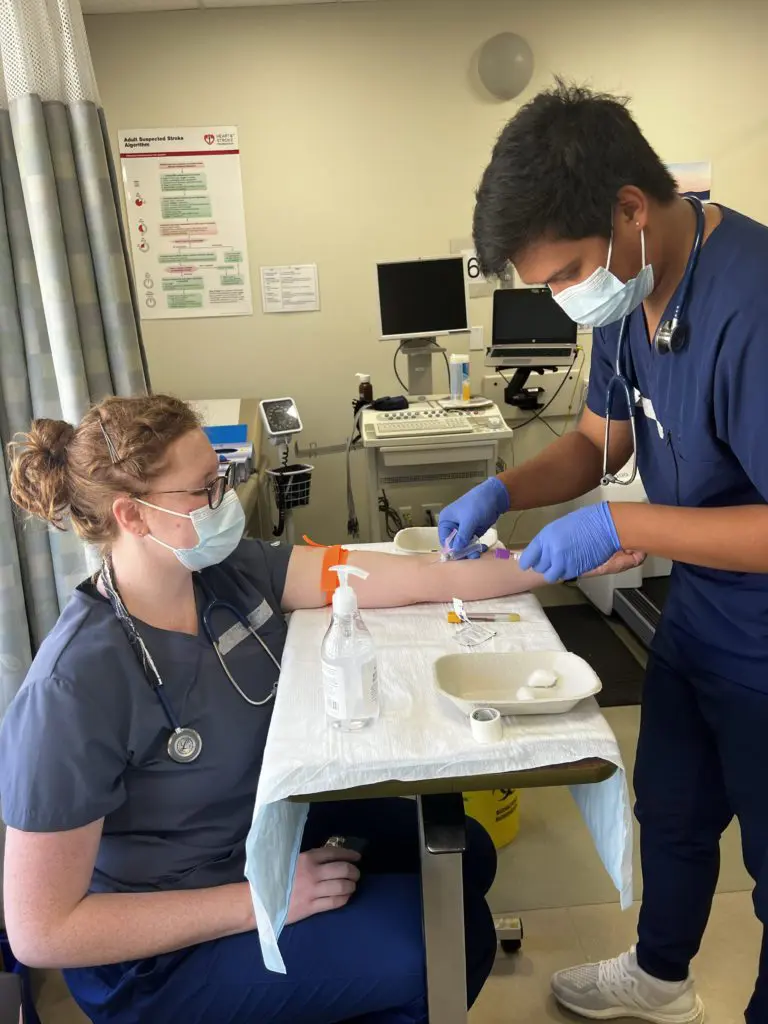
Check out a video of our cardio tech students in action.





![An ECG demonstrates the extensive antero-septal-lateral myocardial infarction [heart attack] that Taryn witnessed.](https://stenbergcollege.com/wp-content/smush-webp/2022/12/ecg-1024x530.jpg.webp)